The power of the human mind coupled with modern technology has the potential to shape healthcare as we know it. The integration of AI in surgery is advancing surgical and procedural medicine to tremendous levels of sophistication.  What does the application of AI in surgery actually look like? What are the powerful capabilities of AI in surgery? How are these cutting-edge technologies used both in and out of the operating room to empower surgeons to improve patient outcomes?
What does the application of AI in surgery actually look like? What are the powerful capabilities of AI in surgery? How are these cutting-edge technologies used both in and out of the operating room to empower surgeons to improve patient outcomes?
Let’s look at four subfields of AI in surgery and how its advancements are increasing precision and predictability in surgical procedures.
The 4 Subfields of AI in Surgery
Artificial intelligence can be broadly defined as "the study of algorithms that enable machines to reason and perform cognitive functions including problem-solving, object and word recognition and decision-making."
Functions like problem-solving, object and word recognition, and decision-making are all integral parts of the surgical process. By training machines to perform these functions, surgical procedures can aid and advance the skills of human surgeons.
There are four main subfields of AI in surgery and each has its powerful applications to enhance surgical and procedural medicine.
1. Machine Learning
Machine learning allows machines to explain or make predictions about data without explicitly programming a desired behavior. Unlike traditional computer programs, machine learning can use data to make predictions by observing patterns.
Machine learning in surgery has powerful implications for surgery as it can identify subtle patterns in large datasets. Using a training dataset of 41,222 patients who underwent craniotomy for a brain tumor, a machine learning ensemble was created that found nonelective surgery, preoperative pneumonia, sodium abnormality, or weight loss, and non-White race were the strongest predictors of increased lengths of stay. Investigators suggest that “machine learning can be applied to a broad range of clinical problems to improve patient care.”
Even more incredible is the potential for machine learning to learn task-agnostic representations of surgical gesture through cross-modal training from video to kinematics and how the learned representations are semantically meaningful even for gestures not contained within the training set. While this is important, the future could be that these approaches become powerful enough to enable a universal technology that tracks surgical progress in real-time, giving feedback regarding possible mistakes, surgical scene depth, next gesture suggestion, etc. with a high accuracy.

2. Natural language processing
Natural language processing advances a computer’s ability to understand human language for large-scale analyses. Natural language processing systems incorporate semantics and syntax into their analyses to successfully understand human-level language.
This form of AI enables machines to interpret meaning from unstructured data. This allows clinicians to record patient data with less rigidity rather than having to input specific text or choose from limited menus. A real-world application of natural language processing is its ability to analyze electronic medical records to predict potential infections in patients.
For example, natural language processing can identify words and phrases in clinical notes for extracting kidney stone composition from large-scale electronic health records. Investigators created a pattern-matching method called StoneX that achieved a positive predictive value >90% for calcium oxalate monohydrate, calcium oxalate dihydrate, hydroxyapatite, brushite, and struvite … and survival analysis from a second stone surgery showed statistically significant differences among stone types.
3. Artificial Neural Networks
Inspired by the biological nervous system, artificial neural networks process signals in layers of computational units, also known as neurons. Neurons are then parameterized by weights that change as the network understands the varying input-output maps that relate to tasks like image recognition or data classification.
When applied to cochlear implant technology, neural networks can be used to assist by correlating data across geometric scales. For example, the inner ear anatomy is at a geometric scale that cannot be routinely acquired with clinical imaging for the purposes of guiding a physical implant. As a result, investigators came up with an approach that translated a high resolution atlas with appropriate anatomical classifications to a patient’s specific clinical cochlea-electrode deployment needs.
The heart of this method used neural networks and achieved a 99.5% classification accuracy and an average localization error of 3.45 mm for 7 landmarks around each inner ear. Advances like this fundamentally enable new workflows that were not possible under normal clinical protocols.
4. Computer Vision
Computer vision refers to machine understanding of images and videos with human-level capabilities. Computer vision is especially vital in computer-aided diagnosis, image-guided surgery and virtual colonoscopy.
For example, one minute of high-definition surgical video is estimated to contain 25 times more data than a high-resolution computer tomography image. The abundance of data could open clinicians to a vast amount of actionable data.
Even more intriguing, investigators have been looking at computer vision methods to survey the ongoing surgical scene during breast lumpectomy to monitor tissue deformations as well as the positions of instruments to improve image-guided navigation systems. The potential of such capabilities is to improve the localization of cancer to increase the likelihood of single-pass surgeries and limit reoperations.
This type of proactive analysis by AI can prevent mistakes or detrimental events during the procedure before they even occur.
The Future of Surgery: What is Next for AI in the Operating Room and Beyond?
The future of surgery will continue to integrate the ever-evolving and maturing technology of artificial intelligence. The integration of AI in surgery can improve procedures at the different stages: preoperative, intraoperative and postoperative.
Each boasts its unique benefits, but all work for the best patient outcome possible. Below are three predictions we may see AI advance and elevate surgery in the future:
Prediction #1: Better Operative Planning with Automated Analysis
We will likely see a rise in patients uploading preoperative data from mobile applications that sync directly to their electronic medical records (EMR). Such data can provide surgeons with a more patient-specific risk for operative planning and provide better predictors for postoperative care.
Prediction #2: Ability to Avoid Adverse Events Intra-Operatively
In the near future, surgeons may be able to execute decision-making intraoperatively based on real-time analysis powered by AI. This analysis would pull from a combination of EMR data, live operative video, vital signs and instrument tracking. This comprehensive and predictive approach could lead to the avoidance of adverse events in surgery.
Prediction #3: Better Recovery Rates with Post-Operative Monitoring
By combining the pre-, intra-, and postoperative data, clinicians can better predict recovery and anticipate potential complications. Furthermore, we may see patients recording their postoperative data on personal devices. This continued monitoring by clinicians will lead to an overall more patient-centered care model.
Ready to Impact the Future of Artificial Intelligence and Surgery?
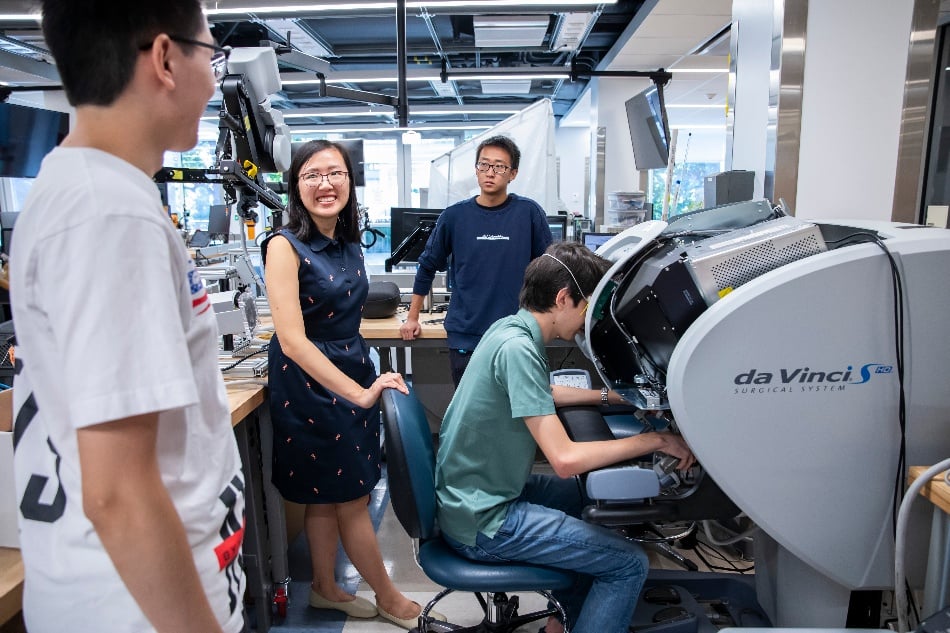
AI in surgery will continue to advance to new heights with the help of highly-skilled engineers. Engineers trained specifically in surgery and intervention will be at the forefront of innovating new solutions using AI.
The master of engineering in surgery and intervention from Vanderbilt School of Engineering is designed to prepare the next generation of engineers to address challenges and envision solutions while utilizing AI at the interface of engineering and medicine.
Michael I. Miga, Ph.D., co-founder of the Vanderbilt Institute for Surgery and Engineering, explains the increased need for professionals in this specialized field in our recent blog post:
"The need for specialized advanced training environments that combine clinical immersion and cutting-edge technology development has never been more pressing."
Are you ready to engineer the path forward to a more patient-specific care model?
If you are interested in further inquiring about our master of engineering in surgery and intervention program, we invite you to request more information.
Want to explore more about Vanderbilt’s master of engineering in surgery and intervention?
)%20(1)-1.png?width=300&name=ESI%20Pillar%20Graphic%20(Instagram%20Post%20(Square))%20(1)-1.png)

.jpg?width=352&name=20181212AR0517%20(1).jpg)

